
Why You’re Stuck: Polyvagal Theory and the Vagus Nerve
Aug 25, 2022Have you ever experienced a gut feeling? Or had butterflies in your stomach before you gave a presentation or speech? This is the mind-body connection in action. Think of the mind-body connection as an information superhighway where messages are communicated on the vagus nerve between the brain and the gut, heart, and lungs (among other areas). In this post, we will discuss the sympathetic vs. parasympathetic states, the vagus nerve and polyvagal theory, and how to stimulate the vagus nerve.
Sympathetic vs. Parasympathetic States
Think about it. Our body processes a lot of information every day. One of the ways that it interprets cues from the outside world around us is by way of the vagus nerve. Information from the gut, heart, and lungs travels to the brain via the vagus nerve and the brain (hypothalamus and pituitary) informs the body how to react. This is how we regulate our autonomic nervous system, which is a fancy phrase for the automatic processes in our body that don’t require our conscious thought. The vagus nerve regulates processes like heart rate, blood pressure, perspiration, and digestion.
Based on our brain’s interpretations of the signals from the body, we can be in three different modes or states:
- Parasympathetic or ventral vagal state
- Our calm state, where we are able to engage, connect, and activate higher learning and focus
- Feelings: Mindfulness, Grounded, Joyful, Curious, Calm
- Bodily responses: decreased heart rate, decreased blood pressure, decreased respiratory rate, increased stomach acid production, increased digestion and motility, circulation to peripheral extremities, increased engagement (“REST AND DIGEST”)
- Sympathetic state
- Our “fight or flight” state, where we feel threatened or in danger, a state where our body seeks to find safety, hyperarousal
- Feelings: Worry, anxiety, panic, fear
- Bodily responses: increased pupil size (you can test this in the mirror!), increased heart rate, increased blood pressure, increased respiratory rate, increased fuel availability, increased blood clotting, decreased immune response, decreased insulin production (MOBILIZATION FOR FIGHTING AND FLEEING)
- Dorsal vagal state
- Our “freeze” state, where we are threatened in such a way that we are immobilized and frozen in place
- Feelings: Burnout, dissociation, shame, helpless, hopeless, numb
- Bodily responses: decreased heart rate, decreased blood pressure, decreased respiratory rate, decreased immune response, increased insulin production (CONSERVING ENERGY, FREEZING)

Polyvagal Theory
As you can see, the body responds to the brain’s perceptions of safety. From investigating the mind-body connection, Dr. Stephen Porges developed the polyvagal theory after realizing that there were two different branches of the vagus nerve, the dorsal branch and the ventral branch. Dr. Porges proposes that the dorsal branch is an older brain circuit. This is the one that supports freezing. Over time, newer brain circuits have developed, creating the ventral branch that supports the ability for you to fight or run away instead of freezing. It makes sense - you’d have greater chances of surviving if you put up a fight against a tiger instead of freezing and playing dead.
The theory also proposes a ladder whereby you can move from a ventral vagal state to the sympathetic state or even the dorsal vagal (freeze) state if under stress. You can move up and down the ladder depending on your stress response from your brain.
Here’s a key point: If your nervous system does not perceive (key word here: PERCEIVE) that you are safe, then your sympathetic nervous system (fight or flight) and the ventral branch are both downregulated (not stimulated) and this allows your dorsal branch to be recruited (activated, stimulated). And what does it promote? Immobilization. Think of soldiers in wartime attacks. Think of domestic violence victims.
Sometimes, people can get stuck in one state, such as a freeze state. But the good news is, there are techniques you can use to move out of the sympathetic or dorsal vagal (freeze) states to the more desired ventral vagal state.
Heart rate variability (HRV): Measuring what state you’re in
You can determine which state you’re in predominantly based on your symptoms, signs (heart rate, respiratory rate, etc..), and assessment of your vagal tone. What is vagal tone? How exactly can you measure vagal tone?
Vagal tone is an assessment of the vagus nerve. Usually, heart rate variability is the best predictor of vagal tone. I’m sure you’ve heard of heart rate variability before but I’ll bet you didn’t realize it was actually measuring if and how your brain interprets you feeling safe. HRV involves measuring the variation in time between each of your heartbeats. A low variation can point to low vagal tone and a more sympathetic dominant state while a high vagal tone (high variation) can point to a more relaxed, ventral vagal state.
While I love people tracking and measuring, I think it’s also important to avoid getting too caught up in the numbers. I’ll see many people change their workout plan based on their HRV numbers irrespective of how they’re actually feeling. Unless you’re a high performance athlete, I feel we lose something when we start ignoring our bodies and focus more on the numbers.. Again, HRV data has a place but I think the numbers should be measured and stacked up against our own cultivated intuition of how our body feels.
![]()
Vagal nerve stimulation
Why would we want to measure HRV or assess vagal tone? For one thing, you can only heal and recover when you are in a ventral vagal state. To promote this state, we can consider vagal nerve stimulation. The implications of vagal nerve stimulation are important for those of you trying to heal from chronic diseases, such as mold toxicity, lyme disease, and other illnesses. Your body has been distressed for so long that it doesn’t trust that it could possibly be safe now. Ensuring that you feel safe, both in mind and body, is vital to restoring balance to your nervous system.
There are two different techniques to vagus nerve adaptation. Some prefer the “top-down approach” where you actually use technique to stimulate the vagus nerve to then send signals to the organs and elicit a change that way. Others prefer the “bottom-up approach” where you utilize diaphragmatic breathing to send a signal to the brain that you are safe and this in turn creates a more ventral vagal response.
Personally, I like to recommend both!
The important takeaway is that you can work to stimulate the vagus nerve and increase vagal tone. This helps to get you out of the immobilization phase and bring you back to a sense of safety. Please consider working with a practitioner, therapist, or other professional if you find that you’re still feeling “stuck” in your trauma or body and mind.
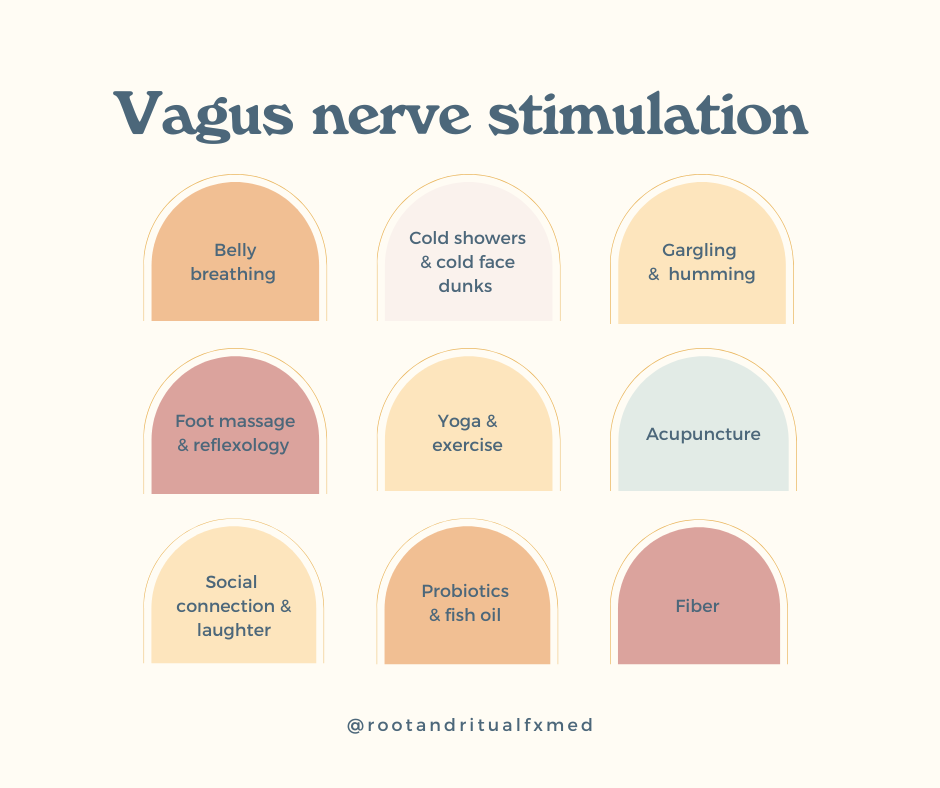
My top 9 techniques for vagal nerve stimulation are:
- Diaphragmatic/belly breathing
- Cold therapy
- Gargling and humming
- Foot massage & reflexology
- Yoga and exercise
- Acupuncture
- Social connection and laughter
- Probiotics and fish oil
- Fiber
As you can see, some of this work relies on the mind and some relies on the body. Some techniques involve supplements while others are more related to social engagement. It’s important to find a way in this busy, hectic world to incorporate vagus nerve stimulation regularly, if not daily.
Personally, you’ll find me rocking the cold showers, trying to laugh, and working on my gut health. Lately, I’m adding more breath work, yoga, and acupuncture to the mix.
If you would like more information on how to support your gut microbiome (which absolutely affects your vagal tone), check out my Essential Guide to Probiotics and Prebiotics!

